AFTER over 18 months of this pandemic, with the social distancing, mask-wearing and on-off lockdowns, what we all want to know more than anything else is when it will all be over and how it will end. While nothing is certain, we have a lot of evidence on which to build some realistic expectations about how the pandemic will progress over the next year or so.

COVID-19 may not be the first time a coronavirus has caused a dreadful global pandemic. It’s been hypothesised that the “Russian flu”, which emerged in 1889, wasn’t actually influenza, but was caused by another coronavirus, OC43.
The Russian flu pandemic caused four or five waves of disease over the following five years, after which it seemed to disappear. In England and Wales, most of the excess deaths it caused were restricted to 1890-91. OC43, the potential cause, still circulates today, though rarely causes severe disease.
Current evidence suggests SARS-CoV-2 – the coronavirus that causes COVID-19 – is also here to stay, a conclusion reached some months ago by many scientists working on the virus. Neither vaccines nor natural infection will stop the virus from spreading.
While vaccines do reduce transmission, they don’t block infection to a high enough degree to eradicate the virus. Even before the delta variant arrived, we were seeing double-vaccinated people both catching the virus and spreading it to others. As vaccines are somewhat less effective at combating delta compared to other forms of the virus, the possibility of infection post-vaccination has grown.

Immunity to infection also starts to wane within weeks of receiving a second vaccine dose. And because immunity to infection is neither absolute nor permanent, herd immunity is unachievable. What this means is that COVID-19 is likely to become endemic, with daily infection rates plateauing depending on how much immunity and mixing there is across the population.
The other human coronaviruses cause repeat infections on average every three to six years. If SARS-CoV-2 ends up behaving the same way, this suggests that in the UK between one-sixth and one-third of people – or between 11 and 22 million – could get infected with it every year on average, or 30,000 to 60,000 a day. But that is not as scary as it sounds.
Yes, emerging research (still in preprint, and so awaiting review by other scientists) does suggest that immune protection against developing symptomatic COVID-19 appears to wane. However, protection against severe disease – generated either by immunisation or natural infection – is much longer lasting. It also doesn’t appear to be lost when facing new variants.
Indeed, for the other human coronaviruses, the vast majority of infections are either asymptomatic or at worst a mild cold. The signs are there to suggest that COVID-19 may end up being the same.
A pandemic with multiple endings
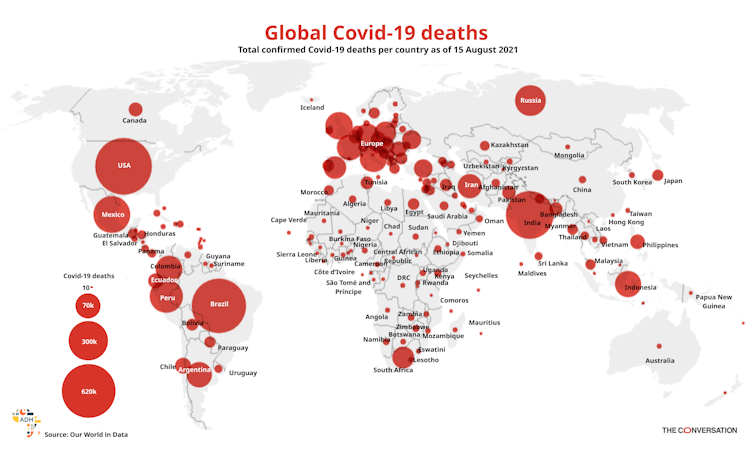
How COVID-19 will end will vary from one country to another, depending largely on the proportion of people immunised and how much infection has occurred (and so how much natural immunity has built up) since the start of the pandemic.
In the UK and other countries with high vaccine coverage and also high numbers of past cases, most people will have some form of immunity to the virus. In England, for example, it’s estimated that at the beginning of September over 94% of the adult population had COVID-19 antibodies.
Among those with prior immunity, it’s been shown that COVID-19 tends to be less severe. And as more people’s immunity is boosted over time by natural reinfections or booster immunisations, we can expect an increasing proportion of new infections to be asymptomatic or at worst cause mild illness. The virus will remain with us, but the disease will become part of our history.
But in countries without much prior illness, even with high vaccine coverage, many people will remain susceptible. Even in countries with the highest vaccine coverage worldwide, over 10% of people are yet to receive a vaccine. Virtually everyone who has not been vaccinated is likely to catch the virus. When infected, they will be as much at risk of severe disease and death (depending on their age and medical status) as at any time during the pandemic.

And in these countries, opening up will almost certainly lead to an exponential growth of infections due to a large number of people with no immunity. And as the amount of virus circulating rises, there will be more cases in vaccinated people too, given that vaccines aren’t 100% protective. Although COVID-19 tends to be less severe in vaccinated people, some do still get very ill – and these countries may see a sizeable number of vaccinated people needing hospital care.
When these countries choose to open up will also have a critical impact. Too soon and many people will still be waiting to be vaccinated. Too late and the effectiveness of vaccines in the already-vaccinated may have started to wane.
Nevertheless, the key lesson from the Russian flu is that COVID-19 will become less relevant over the coming months and that most countries are almost certainly over the worst of the pandemic. But it is still critical that vaccines are offered to the world’s remaining vulnerable populations.
It’s becoming clear that the main impact of vaccination won’t be to stop people from catching SARS-CoV-2 but to reduce the severity of infection the first time people encounter the virus. If people have already been through their first or second natural infection, vaccines will add relatively little protection. To offer the biggest reduction in severe disease, vaccines need to be rolled out to as many people as possible now.
Cecilia Van Cauwenberghe from Frost & Sullivan’s TechVision Group, offers preliminary context about the impact of the COVID-19 pandemic in most African countries, starting with lessons to be learned from previous outbreaks
Different events, such as the Ebola virus disease outbreak in West Africa and the rapid spread of other emerging viruses, including the Middle East respiratory syndrome coronaviruses and the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), exposed a series of limitations in the global infection prevention and control (IPC) programmes. This fact has been severely augmented when combined with an inadequate water supply, poor sanitation and weak hygiene infrastructure in health facilities in various regions, including most African countries.
A team of researchers from the Institute of Global Health at the Faculty of Medicine of the University of Geneva (Allegranzi et al., 2017) focus specifically on this lack of IPC programmes. The study exhibits essential facts about how hospitals and healthcare centres during such outbreaks have become hazardous focal points for patients and medical staff instead of serving the community in safe places where the disease should be controlled and treated. The authors reference a World Health Organization (WHO) communication that emphasises the negative consequences of defective IPC practices during healthcare delivery and how they can harm hundreds of millions of patients worldwide. The analysis, also supported by the evidence of other authors (Holmes et al., 2017), continues with inevitable criticism to healthcare systems exhibiting poor or lacking IPC programmes, followed by some strategies to build strong foundations to reduce the risks and spread of healthcare-related outbreaks.
The situation in most African countries
How to deal with prevalent infectious diseases and access to water, sanitation, and hygiene
Researchers working at the Institute of Community Health, University of Houston College of Pharmacy, Houston, Texas, U.S. (Essien et al., 2021) also highlight knowledge gaps, public health preparedness and research priorities related to COVID-19 infection. Their study focuses on people with HIV/AIDS in Africa and how the onset of the novel virus SARS-CoV-2 that causes COVID-19 threatened Africa’s public health systems. According to the researchers, the challenges faced by most African countries during the pre-existing epidemics, including the highly-rated incidence and prevalence of HIV/AIDS, dramatically increased with the emergence of COVID-19. The authors emphasise the evidence of the outcomes of people with HIV/AIDS with low CD4 cell counts during COVID-19 infection compared to individuals with restored immunity. In addition, they remark the disruption of HIV service delivery in most African countries and need to continue evaluating this particular area of research.
Another remarkable conjunct study presented by researchers from the European Commission–Joint Research Centre in Italy and the Universidad de Granada in Spain (Marcos-García et al., 2021) focuses on the relevancy of the lessons learned from previous outbreaks in Africa. The authors investigate how the incidence of other infectious diseases may increase if most resources are directed to tackle the emergency in the current COVID-19 pandemic context. According to the researchers, the most urgent needs are improving access to water, sanitation, and hygiene (WASH). Although it seems a naïve approach, the lack of these services not only hampers the implementation of preventive measures against SARS-CoV-2 but also connects to high mortality. In this context, the investigators advise about building strategies to explore most African countries’ potential vulnerability to COVID-19, aiming to set strong foundations based on improvements in WASH systems.
Acknowledgements
I want to thank all contributors from the industry involved with developing and delivering this article from Frost & Sullivan.
Further reading
Allegranzi, B., Kilpatrick, C., Storr, J., Kelley, E., Park, B.J. and Donaldson, L., 2017. Global infection prevention and control priorities 2018–22: a call for action. The Lancet Global Health, 5(12), pp.e1178-e1180. Essien, E.J., Mgbere, O., Iloanusi, S. and Abughosh, S.M., 2021. COVID- 19 Infection among People with HIV/AIDS in Africa: Knowledge Gaps, Public Health Preparedness and Research Priorities. International Journal of Maternal and Child Health and AIDS, 10(1), p.113.
Holmes, K.K., Bertozzi, S., Bloom, B.R., Jha, P., Gelband, H., DeMaria, L.M. and Horton, S., 2017. Major infectious diseases: key messages from disease control priorities. Major infectious diseases.
Marcos-Garcia, P., Carmona-Moreno, C., López-Puga, J. and García, A.R.R., 2021. COVID-19 pandemic in Africa: Is it time for water, sanitation and hygiene to climb up the ladder of global priorities? Science of the Total Environment, 791, p.148252.
OVER the past year or so, ordinary people have learnt a lot about viruses, vaccines and the immune system. We have all had to digest a lot of complex specialist knowledge about how safe and effective COVID-19 vaccines are.


But one important – and positive – aspect of the vaccines hasn’t been well communicated. The statistics about COVID-19 vaccine efficacy have only focused on one aspect of immunity: antibodies. But there’s another aspect too: T-cells, a key part of our immune systems. And the good news is that the current vaccines stimulate your T-cells to fight against both the SARS-CoV-2 virus and its emerging variants in the long term.
Let’s recap how the immune system works.
The immune system protects us from various infectious diseases, caused by bacteria, viruses, fungi or parasites. To do this, it first determines what type of infectious agent, or pathogen, is causing the infection. Then it mounts an appropriate response. Crucially, at the same time it produces memory cells that can recognise the same pathogen in future. That sets the immune system up to fight potential reinfections.
If the immune system determines that an antiviral response is needed, it launches a combination of two kinds of immunity. One is mediated by antibodies and the other is mediated by T-cells, or cell-mediated. The antibodies bind to viruses and neutralise them, preventing them from infecting cells. Meanwhile, T-cells kill cells that have already been infected by the virus.
Read more: Coronavirus: B cells and T cells explained
While both kinds of immunity are important in fighting viruses, cell-mediated immunity is far more effective at eradicating viruses and more durable. This is important in the continuing fight against COVID-19.
A powerful weapon
Research has already established that cell-mediated immunity is a powerful weapon against human coronaviruses, the family including SARS-CoV-2. A 2016 study showed that T-cell immunity against the SARS-coronavirus persisted for up to 11 years. It provided complete, effective, and lasting protection against SARS.
Our own recent research argues that a greater focus should be placed on the development of vaccines that are capable of producing antibodies, but would predominantly elicit a cell-mediated immune response against SARS-CoV-2 and its variants.
And, though most people don’t know it, the existing COVID-19 vaccines offer a resilient cell-mediated immune response.
It’s not just about antibodies
The immune system is generally quite effective at eradicating most pathogens. But not everyone’s immune system is equally effective at dealing with the same pathogen; sometimes it needs a little help. Vaccines train the immune system to recognise and respond to a particular pathogen, without first having to be infected by it.
Read more: A brief history of the coronavirus family — including one pandemic we might have missed
Traditionally, most vaccines contain only a small part of the pathogen. This prepares the immune system by mimicking the natural infection.
The current COVID-19 vaccines used in South Africa contain small portions of the wild-type SARS-CoV-2 spike protein – this coronavirus was responsible for the initial COVID-19 outbreak and spread during the early stages of the pandemic.
But, as the pandemic progressed, the virus mutated. Mutations in the spike protein confer certain selective advantages to the virus. Some of these mutations have made the virus easier to transmit, or helped it to escape the immune system. The emergence of variants has raised concerns over the effectiveness of the existing COVID-19 vaccines.
During the course of the pandemic, news reports and press releases have informed on the efficacy and effectiveness of various COVID-19 vaccines against emerging variants. But reports have focused almost exclusively on the ability of the vaccine-induced antibodies, and how effective they are at neutralising the variants.
A resilient cell-mediated immune response
This focus on antibodies means that any news of decreasing antibody efficacy against emerging variants is seized upon as evidence that vaccines may not work well in the long term. This can foster a lack of trust from the public in the science behind the design of COVID-19 vaccines. And this lack of trust could contribute to vaccine hesitancy. After all, some might argue, why take a vaccine that appears less effective against each emerging variant?
In fact, several recent papers have demonstrated that while SARS-CoV-2 variants could escape neutralising antibodies, the cell-mediated immune response induced by most currently used COVID-19 vaccines is very resilient and remained effective.
While antibodies induced by the vaccine were able to bind to the variants, they were less capable of neutralising them. The T-cells, on the other hand, were largely as responsive to the variants as they were to the wild-type virus. They were still able to recognise and respond effectively to the variants, conferring resilient protection against the disease.
To date, only Johnson & Johnson has released a media statement that includes statistics about both kinds of immune responses induced by its vaccine.
Research shows that antibody levels produced from different vaccines decrease over time and, although immunity varies from person to person, immunity from the Pfizer and the Johnson & Johnson vaccines typically last for at least six months.
Build public trust
Vaccine hesitancy is a major hurdle in fighting the pandemic. A recent survey showed that only 72% of South Africans were willing to be vaccinated against COVID-19.
The idea that “the vaccine will be ineffective” was one of the most common reasons people gave for vaccine hesitancy. Hesitancy isn’t surprising if people hear only about how part of the immune response becomes less effective against emerging variants.
Public trust in the vaccine relies on people understanding the complete efficacy of the vaccine-induced immune response and communicating the statistics about both kinds of responses to the variants. The existing COVID-19 vaccines offer a resilient cell-mediated immune response. Knowing this can help people make an informed decision about vaccination.
THERE’S been an increase in COVID-19 deaths across Africa since mid-July 2021. But the impact of the pandemic in sub-Saharan Africa remains markedly lower compared to the Americas, Europe and Asia.



The reasons for this are not yet clear. Several factors have been suggested as potentially influencing the low burden of COVID-19 illness. These include age demographics, lack of long-term care facilities, potential cross-protection from previous exposure to circulating coronaviruses, limitations of SARS-CoV-2 testing which may have resulted in an undercounting of deaths, and effective government public health responses.
In a recent paper our team of public health researchers, led by health analyst Janica Adams, examined these possible explanations by reviewing the scientific literature. The aim was to help guide public health decision making to contain COVID-19.
Common theories
A number of hypotheses emerged from the literature review. In this article, we explore the most common ones. More research is needed to better understand how these factors contribute to the lower burden of COVID-19 disease in the African context.
The young age demographic of sub-Saharan Africa
Age has been observed as a significant risk factor for severe COVID-19 illness. Most deaths occur in those aged 65 or older. The median age in North and South America, Europe and Asia ranges from 32 to 42.5 years. The age demographic structure of sub-Saharan Africa is much younger – the median age is 18.
The stark difference in age demographics can be demonstrated by comparing Canada and Uganda, which are similar in population size. In Canada, the median age is 41.1. Around 18% of the population is 65 or older. In contrast, the median age of Uganda is 16.7. Only 2% of the population is 65 or older. Canada has recorded nearly 1.5 million COVID-19 cases and 27,000 deaths compared to fewer than 100,000 cases and 3,000 deaths in Uganda. COVID-19 has a significant impact on older people. Countries with larger proportions of older people are more likely to be hardest hit.
Lack of long-term care facilities
Most elderly people in sub-Saharan Africa don’t live in long-term care facilities. These facilities pose significant risks for infectious diseases. COVID-19 has substantially affected those living in long-term care facilities. During the first wave of the pandemic, about 81% of deaths in Canada occurred in those facilities.
In sub-Saharan Africa, provision of care is mostly left to families. This limits the number of formal caregivers and thus reduces the chance of transmission. An exception to this is South Africa, which has an established long-term care sector. South Africa was the worst affected country in sub-Saharan Africa. And 33% of COVID-19 outbreaks in South Africa occurred in long-term care facilities during the first wave.
Potential cross-protection from local circulating coronaviruses
It’s been suggested that prior exposure to circulating coronaviruses could reduce the severity of COVID-19 illness if people have developed antibodies. A previous study demonstrated that prior exposure to endemic coronaviruses resulted in lower chance of death and lower disease severity compared to those who were not previously exposed. Human-bat interactions are common in some rural areas of Africa.
Limitations of SARS-CoV-2 testing
There are concerns that the limited SARS-CoV-2 testing may have resulted in an undercounting of COVID-19-related deaths in sub-Saharan Africa. Insufficient data collection may mean we don’t really know the incidence and prevalence of COVID-19. Though varying across sub-Saharan Africa, testing levels have been low compared to other areas of the world.
Effective government public health response
The rapid response of several African governments and health organisations may have played a significant role. At the beginning of the pandemic, several measures were taken: screening, establishment of the Africa Task Force for Novel Coronavirus, suspension of flights from China and closure of borders in 40 African nations. New programmes also promote sharing of COVID-19 information across sub-Saharan Africa.
In contrast to high-income countries which focus on non-communicable diseases, health organisations in sub-Saharan Africa focus on infectious diseases. The formation of national public health institutions has been key in curbing infectious diseases in Africa through disease surveillance, diagnostics and rapid response to outbreaks.
But stringent lockdowns have taken a serious economic and societal toll across sub-Saharan Africa. Lockdowns resulted in increased food insecurity, teenage pregnancy, gender-based violence, and disruptions in the treatment of malaria, TB and HIV. Africa’s 54 nations are not all the same, and local responses should be tailored to the health, social and economic realities in specific countries.
South Africa: the outlier
In contrast to the rest of sub-Saharan Africa, South Africa has experienced higher proportions of COVID-related hospitalisations and deaths. South Africa has a remarkably higher median age and a long-term care sector. In addition, the higher rates of HIV and TB in South Africa have been associated with higher COVID-19 death rates. The prevalence of non-communicable diseases in South Africa is higher than in other regions, which may contribute to the higher burden of COVID-19 disease. South Africa also has better diagnostic capabilities and healthcare documentation than other sub-Saharan African countries. This may contribute to higher reporting rates.
Recommendations
We believe that the low median age and a small percentage of vulnerable elderly contribute significantly to sub-Saharan Africa’s lower COVID-19 death rates.
Based on our research, we propose several policy prescriptions to help improve health practice.
Lockdowns lead to severe health consequences for the young and the poor in the African context. Therefore, reduced emphasis on lockdowns should be considered.
Better communication with the public is required to help curb COVID-19.
Governments should find adequate financial support for vulnerable sectors, possibly from external agencies.
Governments and health agencies should ensure that medical infrastructure is available in the case of a severe outbreak, as seen with the oxygen shortage in India.
International efforts should prioritise developing vaccines that are effective against virus variants of concern and ensuring equitable access to such vaccines.
The emergence of variants of concern with increased potential for transmission and more severe disease in the younger population could make Africa more susceptible to a severe COVID-19 epidemic. These variants need to be monitored through molecular epidemiologic surveillance. And further studies are needed to better understand potential mechanisms of severe disease in the African context.




