AS Britain announces its roadmap out of lockdown, vaccine certificates have once again come into the spotlight.
British Prime Minister Boris Johnson said there would be a review into the issue although he added some form of vaccine passport would be “going to come on the international stage whatever” for foreign travel.
Governments and developers around the world are exploring how certificates and passports could help to reopen economies by identifying those protected against COVID-19.
Proponents say identifying people who are immune to the novel coronavirus or at lower risk of spreading it could help open up travel and other services. But, critics have raised concerns over privacy, health and discrimination.
As more technology firms develop digital certificates that can be accessed on smartphones by employers, airlines and others, here is all you need to know about health passports.
WHAT ARE HEALTH PASSPORTS?
The term health passport, or health pass, generally refers to documents – in paper or digital format – that certify a person is unlikely to either catch or spread a disease.
With the novel coronavirus, the proposed certificates would attest one of three things: that the holder has been vaccinated, has tested negative for the virus or has recovered from it.
Their use could allow governments to lift some pandemic-induced restrictions, allowing people to travel in planes, attend concerts, go to work or dine out, supporters say.
“We’ve tried many different solutions to properly and safely reopen hospitality, sport venues and other things that are very important, not just for our economy, but also for mental wellbeing of people,” said Ryan Wain, an advisor at the Tony Blair Institute for Global Change, a British think tank.
“And really, the only way that we can properly get those open is knowing that people entering those venues don’t have COVID,” he told the Thomson Reuters Foundation in a phone interview.
WHERE ARE THEY BEING USED?
Different health passes have been trialled by governments and firms around the world in recent months.
Tech giants including Microsoft Corp , Oracle Corp and healthcare companies Cigna Corp and Mayo Clinic in January become part of a coalition pushing for digital records of people who get vaccinated against COVID-19.
The project, called Vaccination Credential Initiative, aims to help people get encrypted digital copies of their immunization records stored in a digital wallet of their choice.
Bahrain launched a digital COVID-19 vaccine passport in February, one of the first countries to do so.
Denmark has said it would launch an initial version of a coronavirus vaccination passport by the end of February, while Sweden plans to launch a vaccine passport by summer.
Last October, Estonia and the World Health Organization started a pilot for a digital vaccine certificate.
Meanwhile, China has put in place an app-based health code system that uses travel and medical data to give people a red, yellow or green rating indicating the likelihood of them having the virus – and whether or not they can walk around freely.
Israel has said it plans to issue a “green passport” to those who have been vaccinated, which will grant them easy access to restaurants and cultural events, and exempt them from quarantine rules or getting a virus test before travel.
Last April, Chile said it would issue certificates to people who recovered from the virus.
And in India, everyone who has been vaccinated will get a QR code-based electronic certificate, the health ministry has said.
At a smaller scale, the University of Illinois has made access to campus buildings dependent on negative tests, and a number of airlines have started trialling a digital health pass to verify tests taken in different countries.
The International Air Transport Association, the lobby group of the world’s airlines, said it would launch a digital health travel pass in 2021 that will include passengers’ COVID-19 vaccination data.
British Airways has said it would trial a mobile health app that combines travel verification documents and COVID-19 test results to ensure passengers are compliant with destination entry requirements.
The app is already being used by American Airlines.
WHAT ARE THE MAIN CONCERNS?
Health passes have raised a number of public health and privacy concerns.
Legal and health experts have warned that so-called immunity passports, which would allow greater freedom to those who have recovered from the virus, could push people to try to catch the disease in the hopes of making themselves immune.
The passports’ scientific grounding has also been called into question, as it is still not clear whether people who recover from COVID-19 are protected from a second infection – or, if they are, for how long.
Passes based on negative test results have a short shelf life, as people can catch the virus any time after taking the test, said Alexandra Phelan, an infectious disease expert at Georgetown University in Washington, D.C.
The passes also rely on wide access to rapid testing, she added.
Phelan noted that vaccination certificates are already regulated by international law, which allows countries to require from travellers proof of vaccination for diseases such as yellow fever or polio as a condition of entry.
But extending the system to COVID-19 might face some hurdles, as governments have to agree on which of the several vaccines in the pipeline they would accept, she said.
With researchers warning that it might take years to get everyone a shot as rich nations buy up more than half of the available stock, linking travel to a vaccination could also leave a large part of the world grounded, Phelan added.
“We risk a situation where only wealthy countries have had access to the vaccine that is accepted for travel. And they’re the only ones travelling,” she said.
WHY DIGITAL AND NOT PAPER?
Certificates could in theory be paper-based or digital, but trials have largely focused on digital solutions.
Inequitable access to the COVID-19 vaccine could incentivise people to falsify papers, said Phelan.
And paper documents are inherently easier to forge, added Nick Page, product director at Onfido, a British tech company working on health passports.
But apps and other digital solutions combining health data and identification could exclude large numbers of people who do not own a smartphone, while also raising privacy concerns, said Tom Fisher, a researcher at nonprofit Privacy International.
“Digital identity solutions leave us open to data exploitation, with the valuable data from these solutions (being) used for other purposes,” he said in an email.
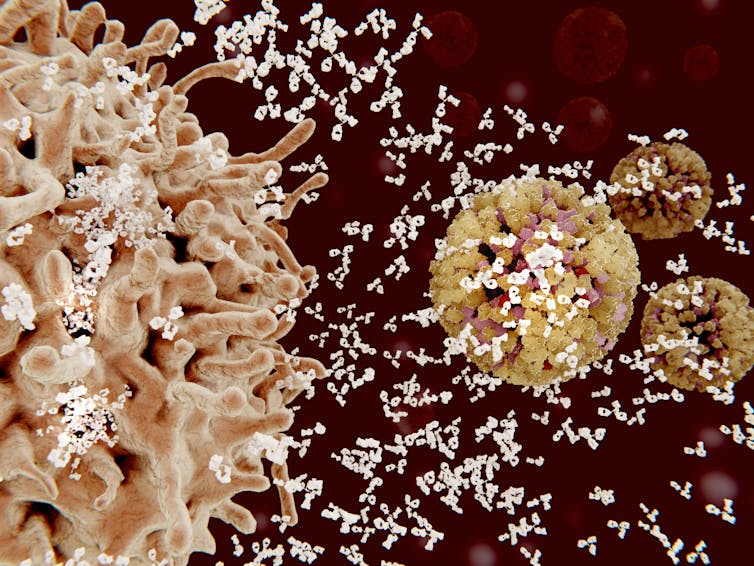
THE goal of the COVID-19 vaccines being rolled out worldwide is to stimulate our immune systems into creating a protective response against the coronavirus, particularly by generating antibodies. These antibodies then circulate in our blood until needed in the future, attacking and removing the coronavirus quickly from our bodies if we become infected.

The speed with which the scientific and medical communities have developed and tested these new vaccines has been extraordinary. However, this short timescale leaves us with some outstanding questions.
Key among these is how long the protection we receive from vaccination, or indeed from infection with the virus itself, will last. We know, for example, that antibody levels drop quite quickly following a COVID-19 infection.
How the immune system remembers
Our body’s remarkable ability to remember past encounters with infectious microorganisms and retain robust defences against them is due to the phenomenon of immunological memory. This memory resides in white blood cells known as lymphocytes, of which there are two main types: T cells and B cells.
When the body faces a new challenge – either a new infection or vaccine – specific T cells and B cells are recruited to deal with it. “Memory” versions of these specific cells are then kept on standby in case the same issue is encountered again in the future.
It is these B cells that are responsible for releasing antibodies into the blood. When an infection or vaccination occurs, some of them will metamorphose into specialised antibody-production factories, known as plasma cells.
Antibodies are proteins, and like any other protein will be naturally broken down and removed from the body within a few months at most. This is the reason why protection from antibodies that we receive passively, for example from our mothers in the womb or through breast milk, does not last very long. For longer-term protection, we need to produce antibodies for ourselves.
Our body’s ability to maintain antibody levels following infection or vaccination is a result of two mechanisms. In the early stages, if memory B cells detect any persistent infection or vaccine, some will continue to turn into new antibody-producing plasma cells.
Once the infection or vaccine has been completely removed, memory B cells no longer replenish the plasma cell population, which declines. However, some may persist as long-lived plasma cells (LLPCs), which can live for many years in our bone marrow, continually manufacturing and releasing large quantities of antibodies. LLPCs aren’t always created after an infection, but if they are, antibodies against a specific infection can be found in the blood for a long time after the infection has cleared.
Although we don’t yet fully understand which immunisation conditions are best for generating LLPCs, their presence has been linked to certain locations. For example, a US group discovered that LLPCs appear to prefer the marrow of certain bones above others. Ten years after tetanus vaccination, LLPCs were found in femur, humerus and tibia bone marrow much more commonly than that of the ribs, radius, vertebrae or iliac crest.
Quite why LLPCs prefer the marrow of these bones is not yet clear. One interesting possibility is differences in the bone marrow fat level. LLPCs were found to be surrounded by large numbers of fat cells in these bones. This suggests that it may be bone marrow fat content that affects the ability of LLPCs to move to – and reside long term in – certain bones.
But if LLPCs aren’t created, that doesn’t mean someone cannot generate more antibodies against a threat if it is encountered again in the future. Providing the person has generated memory B cells, these will recognise the familiar threat, and once again some will start transforming into new plasma cells, to begin antibody production once more.
Vaccine type affects durability too
There are many reasons why vaccination or infection do not always provide protection that is long lasting. Some of this is due to individual variation in our response to a given vaccine. However, the features of vaccines themselves determine the nature of the antibody response too.

One study found that although a greater proportion of individuals who received tetanus and diptheria vaccines developed protective antibodies, these antibodies faded more rapidly than those generated by measles, mumps or smallpox vaccines. The key difference between these vaccines is that those against tetanus and diptheria contain only isolated proteins (modified versions of the toxins that tetanus and diptheria bacteria make), whereas the measles, mumps and smallpox vaccines contain live, weakened versions of these viruses.
Some people may not produce good responses to live vaccines due to pre-existing immunity to the vaccine itself, having already had a natural infection. However, those that do respond well tend to keep their responses for longer. This is partly due to persistence of the live vaccine in the body, which encourages the short-term replenishment of plasma cells. It is also likely that live vaccines are better at producing LLPCs.
We have already seen that the rate at which antibodies decay following COVID-19 can differ, for example between men and women. Many of the new COVID-19 vaccines are based on novel delivery methods, such as viral vectors or messenger RNA molecules. Clearly these are very effective in their delivery of rapid protection. But quite how well they will activate memory B cells and LLPCs, imparting long-lived immunity, remains to be seen.
SOUTH African natural gas and helium producer Renergen will start production of its helium powered ultra-cold mobile freezer in the next few days and has started discussions to sell the units to logistics companies, it said yesterday.
Companies and governments around the world are working on ways to establish cold-chain storage and delivery systems for vaccines such as the Pfizer Inc and BioNTech shot, which must be shipped and stored at ultra-cold temperatures and can only last at standard fridge temperatures for up to five days. As a solution, Renergen on Monday launched its prototype cold-chain storage called Cryo-Vacc, which has a temperature range of -150 degrees Celsius to 8C and can store vaccines for periods of up to 30 days without the need for any power supply.
“We’ve already started to take orders for this product. So we’re ready to start going into production in the next few days,” Renergen CEO Stefano Marani told journalists at the demo-launch event.
The company has partnered with local distributor DPD Laser, jointly owned and controlled by The Laser Group and European DPDgroup, which will buy the units from Renergen and then rent them out to its healthcare warehousing and logistics clients in South Africa and the Southern African Development Community (SADC).
Marani said the company had also received multiple expressions of interests and order requests from all over the world.
Cryo-Vacc uses liquid helium to transport by air, and liquid nitrogen to transport by road. Current cold-chain solutions use dry ice – frozen carbon dioxide – or cold plates, but this has not been sustainable for South Africa said DPD Laser CEO Anton Visagie.
“Our biggest challenges … we’ve got very high ambient temperatures in South Africa, we’ve got long distances to travel and often when you get to the point of vaccination there is a lack of infrastructure. There could be load shedding,” he said referring to frequent scheduled power cuts.
Another difficulty with vaccine transport is that aircraft can only carry a limited amount of dry ice as it turns into gas over time, displacing the breathable air in the cabin.
Marani said because liquid helium is only a fraction of the weight of liquid nitrogen, it will significantly reduce airfreight distribution costs and can accommodate up to 12 times more vials per flight compared to other solutions based on current flight safety regulations.
Earlier this month the health ministry called for bids from service providers to import, store and distribute COVID-19 vaccines at different required temperatures.
South Africa has yet to launch its COVID-19 vaccination programme and the government has decided to go with the Johnson & Johnson’s dose after trial results this month showed AstraZeneca’s two-shot vaccine was less effective against the new variant of the coronavirus dominating South African infections.
Source – Thomson Reuters Foundation
African countries may suffer in the global rush for vaccines because they are unable to gather statistics that reveal the true extent of the spread of Covid among their populations, epidemiologists and other experts fear.
According to data from Johns Hopkins university, there have been 3.7m confirmed cases in Africa, and the landmark figure of 100,000 confirmed deaths is likely to be reached within days.
A series of studies has raised fears that the official figures are a significant underestimate, raising the possibility that Africa may not be seen as a priority for scarce global vaccine supplies despite the urgent need.
Many African countries are unable to afford mass testing and lack the capacity to collect reliable data on cases and deaths, especially in remote areas. The stigma attached to the disease, a lack of information and victims’ inability to either reach or pay for health facilities may also reduce reporting.
The World Health Organization has said the “unique socio-ecological make-up in a number of African countries means a slower rate of transmission, and fewer severe cases as compared to the hardest-hit countries”.
Mortality rates have been relatively low across Africa compared with other regions, though they are rising.
Dr Oliver Watson, an infectious disease expert at Imperial College London, said the shortcomings in data collection on the continent could undermine efforts to secure equitable access to vaccines.
“Some might argue the need for vaccines is much less urgent … so the vaccines will go to countries with stronger reporting systems and so further entrench inequity,” he said.
A study by scientists from ICL’s Covid-19 response team in Sudan found that only about 2% of Covid deaths had been reported in the capital, Khartoum, through most of last year. As a result, the team estimated that as many as 16,090 deaths may have been unaccounted for as of 20 November. Sudan has officially recorded fewer than 30,000 cases and 1,849 deaths.
According to UK Sudan’s Doctors’ Association, 40 doctors are thought to have died of Covid in the country between March and January. As of 6 February, 1,107 health staff had been tested for Covid with 76% returning a positive result.
Dr Ibrahim Fahal, the president of the UK-based Sudan Medical Care Foundation, said frontline medical staff faced acute shortages of PPE, limited safety measures and very large numbers of patients. “They are very exposed,” he said. “A way to get them vaccines has to be found and as soon as possible.”
A study by the Boston University School of Public Health in Zambia concluded that Africa’s relatively low numbers of Covid cases might simply be “a matter of lack of testing, with the coronavirus actually taking a terrible but invisible toll across the continent”.
The study, which is expected to be published in the British Medical Journal in the coming days, found that more than 15% of recently-deceased people arriving at the main morgue in the capital, Lusaka, over the summer tested positive for Covid. Despite most having had symptoms, few were tested before death.
“Our findings cast doubt on the assumption that Covid-19 somehow skipped Africa or has not impacted the continent as heavily,” said co-author Lawrence Mwananyanda. “This study shows that with proper diagnostics and testing, we can begin to identify the scale of Covid-19 in African countries such as Zambia.”
The most recent excess mortality figures in South Africa reveal 137,000 extra deaths since May last year, of which a high proportion can be attributed to Covid-19, experts say. The official Covid death toll stands at 47,382.
Only a handful of serological studies have been conducted in Africa compared with Europe, the Americas or South Asia, but these also point to a much wider spread than official figures suggest.
One in Kenya showed that by the end of July 2020, when the country had reported only 341 deaths and 20,000 cases, around one in 25 blood donors in several locations had been infected.
The low number of deaths was explained by demographics in Kenya, where less than 4% of the population is 65 or older, a factor which may also help explain the relatively low death rates across the continent.
Official figures do not include Tanzania, a country of nearly 60m, which has not reported official statistics since April, when it logged 509 cases. Its president, John Magufuli, has disparaged vaccines and said Christian faith will protect the country.
The US embassy in Dar es Saleem said in a statement on Thursday that it was aware of a “significant increase in the number of Covid-19 cases since January”.
Anecdotal evidence also suggests much higher numbers than reflected in official statistics in neighbouring Zimbabwe, which has officially recorded 35,000 cases and 1,364 cases.
Gravediggers and undertakers in Harare’s Warren Hills cemetery, however, describe an unprecedented number of deaths.
Ewing Ishemunyoro said he had been digging six graves a day since January, three times the previous average. “It is clear the authorities do not want people to know that there are more Covid burials, but it is happening and we see that every day,” he said.
Only a handful of African countries believe they will be able to immunise their frontline health workers over coming months, and the vaccination of general populations may not be completed for several years, leaving hundreds of millions of people vulnerable.
African health facilities have struggled to cope with the second wave of infections across much of the continent, fuelled by new variants of the virus. Two-thirds of the 21 countries the WHO surveyed reported inadequate critical care capacity and more reported a shortage of oxygen in recent months.
The WHO’s regional director for Africa, Dr Matshidiso Moeti, said last week: “The increasing deaths from Covid-19 we are seeing are tragic, but are also disturbing warning signs that health workers and health systems in Africa are dangerously overstretched.”
The WHO said it had repeatedly made clear that their statistics for the continent showed reported cases and that only seroprevalence studies could reveal the actual burden.
“It is important that we do not allow pre-conceived biases about Africa to cloud our understanding of what is happening in the region.
“Transmission and mortality are lower than what we see in other hard-hit countries, but the fragility of health systems necessitates a strong response. We have no evidence to the contrary.”
Additional reporting by Nyasha Chingono in Harare
Source - The Guardian UK




